Clinical Research Guidelines and Tools
Clinical research can be categorized into:
- Interventional Studies (Clinical Trials): Research involving participants who receive specific treatments or interventions to evaluate their effects.
- Observational Studies: Studies that assess health outcomes in groups of people without assigning specific interventions (e.g., epidemiological studies, cohort studies).
- Behavioral and Public Health Research: Investigating how behaviors, social factors, and public health initiatives influence health outcomes.
Clinical research follows ethical and regulatory standards to protect participants, ensure data integrity, and contribute to evidence-based medicine and public health policies.
The Office of Research & Innovation (ORI) continues its efforts to provide best practices, enhance collaboration, and reinforce our commitment to Drexel University and our Research Community. As part of these initiatives, ORI is releasing an initial set of Clinical Research Guidelines and Tools to encourage best practices in line with applicable regulations, procedures, and Good Clinical Practice (GCP). Additionally, future guidance and resources are also mentioned, including both Drexel and Non-Drexel resources. Non-Drexel resources are available for reference but should be assessed prior to use based on the specifics of the project and other applicable regulatory requirements as well as University policies, procedures, and requirements. These resources will be updated and expanded throughout 2025 and 2026.
Please note that your funder or sponsor may have different templates or forms that are required to be used, so please refer to the terms and conditions of your award.
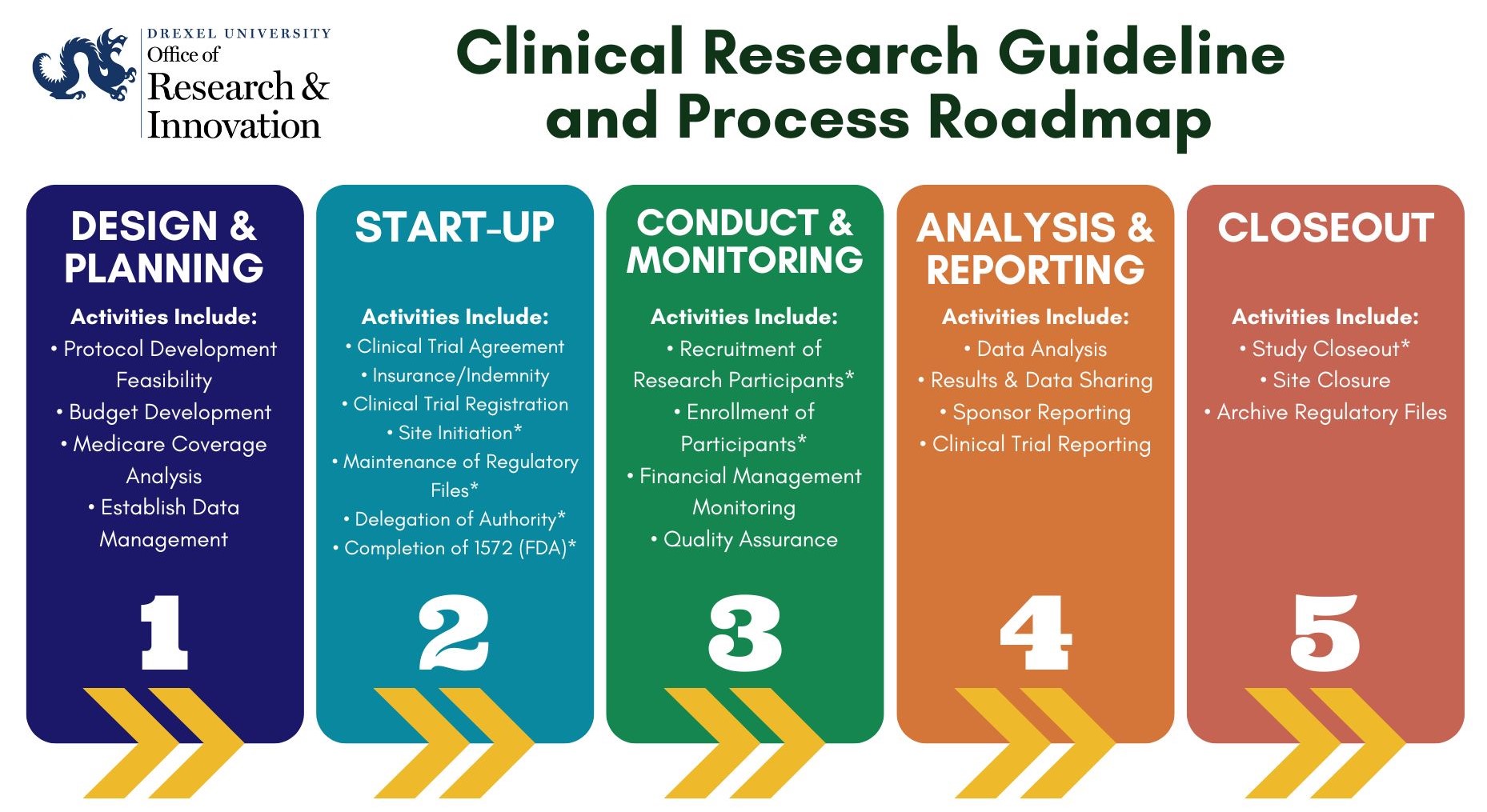
View the text version of the Clinical Research Guideline and Process Roadmap
Step 1: Design and Planning
Future guidance and resources include: Feasibility, Budget Development, Medicare Coverage Analysis.
Step 2: Start-Up
In addition to the below, future guidance and resources include: Clinical Trial Agreements, Insurance/Indemnity, ClinicalTrials.gov Registration.
- ORI-613 Guidelines for Site Initiation [PDF]
- ORI-615 Maintenance of Regulatory Files [PDF]
- ORI-616 Delegation of Authority [PDF]
- ORI-617 Completion of Form FDA 1572 [PDF]
- Training (e.g., GCP, Human Subjects, RCR)
- Human Research Protections/IRB
- Conflicts of Interest (COI)
- Sponsored Programs
- Contracts and Budget Submission
- Data Use Agreements
Step 3: Conduct and Monitoring
During a clinical research study's conduct and monitoring step, ongoing oversight ensures that the study adheres to the protocol and regulatory requirements. Regular monitoring visits and data reviews are conducted to verify the accuracy and completeness of collected data, participant safety, and compliance with requirements; this includes any data safety monitoring boards or plans being completed as required or approved. Any deviations, adverse events, or issues are documented, addressed promptly, and reported to the IRB, funding agencies, or others as required. Monitoring also includes checking the informed consent process, ensuring proper management, and maintaining the integrity of regulatory files. These activities help ensure the trial’s quality, participant safety, and reliable outcomes.
In addition to the below, future guidance and resources include: Monitoring, Financial Management, ORI Quality Assurance.
Step 4: Analysis, Reporting, and Publication
The analysis and reporting step involves evaluating the study data to assess treatment safety and efficacy. Based on the study plan, statistical analysis is conducted, focusing on primary and secondary endpoints. Results, including any adverse events, are compiled and shared with stakeholders, regulatory bodies, and the scientific community. This ensures transparency and contributes to medical knowledge.
Future guidance and resources include: Clinical Trial Reporting and Data Sharing.
Step 5: Closeout
In addition to the below, future guidance and resources include: Research Document Retention and Disposal.